Podcast: Embed
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | Pandora | iHeartRadio | Blubrry | TuneIn | Deezer | RSS
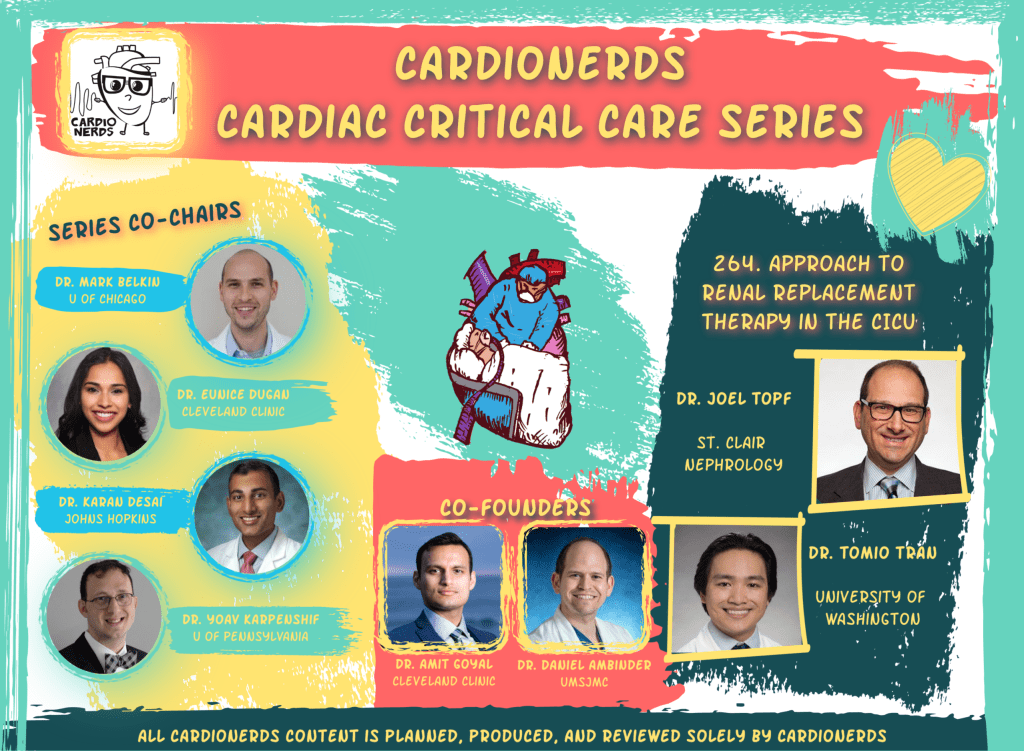
Renal replacement therapy (RRT) is routinely utilized in the CICU. Series co-chairs Dr. Eunice Dugan and Dr Karan Desai along with CardioNerds Co-founder Dr. Daniel Ambinder were joined by FIT lead and CardioNerds Ambassador from University of Washington, Dr. Tomio Tran. Our episode expert is world-renowned nephrologist Dr. Joel Topf. Dr. Topf is Medical Director of Research at St. Clair Nephrology, and editor of the Handbook of Critical Care Nephrology. In this episode, we describe a case of cardiogenic shock due to acute myocardial infarction resulting in renal failure, ultimately requiring continuous RRT (CRRT). We discuss the most common causes of AKI within the cardiac ICU, indications for initiating RRT, evidence on the timing of RRT, different modes of RRT, basic management of the RRT circuit, and how to transition patients off of RRT during renal recovery. Episode notes were drafted by Dr. Tomio Tran. Audio editing by CardioNerds Academy Intern, Dr. Maryam Barkhordarian.
The CardioNerds Cardiac Critical Care Series is a multi-institutional collaboration made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Mark Belkin, Dr. Eunice Dugan, Dr. Karan Desai, and Dr. Yoav Karpenshif.
This episode is made possible with support from Glass.Health – The first digital notebook designed for doctors. Follow @GlassHealthHQ for the latest product updates!
Pearls • Notes • References • Production Team
Pearls and Quotes – Approach to Renal Replacement Therapy in the CICU
- Do not commit “Renalism” – withholding lifesaving treatments from patients with renal impairment due to fear of causing renal injury. Shared decision making is key.
- In the ICU, most of the time, AKI is caused by ATN due to adverse hemodynamics. Nephrologists can help determine the cause if the patient has an atypical presentation.
- Late dialysis initiation is non-inferior to early dialysis initiation. Early initiation may lead to higher rates of prolonged time on dialysis.
- Slow low efficiency daily diafiltration (SLEDD) vs CRRT are equivalent in terms of outcomes and are the preferred methods among patients with hypotension. Intermittent Hemodialysis (iHD) can be used once patients are hemodynamically stable.
- A “Furosemide Stress Test” can be used to test intact renal function or renal recovery by challenging the nephron to make urine.
Show notes – Approach to Renal Replacement Therapy in the CICU
What are the risk factors and differential for AKI in the CICU?
- Start by using the pre-renal vs intrinsic renal vs post-renal framework. Additional considerations in cardiac patients include contrast induced nephropathy, pigment nephropathy, cardiorenal syndrome. Enjoy Episode 262. Management of Cardiorenal Syndrome in the CICU.
- In the ICU setting, intrinsic renal injury due to ATN is among the most common etiology of AKI.
- Many risk factors for AKI are not modifiable in the ICU. Optimize renal function by avoiding nephrotoxins, minimizing contrast usage, and keeping the MAP >65-75 mmHg.
- Contrast nephropathy as an etiology is questionable and may be a marker of a sicker patient population. Avoid “Renalism” – providing substandard care to patients with renal disease due to fear of worsening renal function.
- Most etiologies are treated with supportive care.
What is the approach to timing of renal replacement therapy initiation?
- Definitions for early vs late vs very late initiation of RRT:
- Early – Worsening AKI without indications for RRT
- Late – Worsening AKI with relative indications for RRT
- Very late – Worsening AKI with strict indications for RRT
- Late initiation is noninferior in terms of mortality; early initiation is associated with higher rates of prolonged/permanent RRT.1,2,3
- Very late initiation associated with worse outcomes.4 In general, start RRT if there are absolute indications (“AEIOU) or the patient is anuric with a high BUN (~140) as delaying RRT much further is associated with worse outcomes.
- “Furosemide Stress Test” (FST) can be used to predict RRT need.5
- 1 mg/kg IV for diuretic naive, 1.5 mg/kg IV if on diuretic
- Goal = 200 cc urine over 1-2 hours
For the non-nephrologists, what are options for RRT acutely and how do they work?
- There are two principles of RRT:
- Convection – movement of solutes through semipermeable membrane using pressure
- Ultrafiltration – volume removal using convection; fluid is then replaced to prevent hypovolemia
- Fluid removed has the same composition of the plasma
- Negative fluid balance is the difference between volume removed and replacement fluid; goal usually 25-250 cc/hour
- Ultrafiltration – volume removal using convection; fluid is then replaced to prevent hypovolemia
- Diffusion – movement of solutes from high to low concentration
- Dialysate runs countercurrent through semipermeable membrane
- Typical dialysate composition – normal sodium, magnesium, low potassium, no creatinine, no BUN, high bicarbonate
- Does not remove fluid
- Convection – movement of solutes through semipermeable membrane using pressure
- There are 3 types of RRT: iHD (intermittent hemodialysis), CRRT (continuous renal replacement therapy), SLEDD (slow low efficiency daily diafiltration)
- None have been shown to be superior in normotensive patients
- iHD can remove potassium and toxins more quickly
- SLEDD and CRRT are equivalent and preferred for hypotensive patients.6
- SLEDD is less labor intensive
- Institutions usually have a preference of one modality over another
- Peritoneal dialysis has been used in the ICU in some specialized centers, but is not common.
- There are 3 methods of CRRT:
- Continuous hemodialysis
- Removes fluid by diffusion
- Uses dialysate, no replacement fluid
- Removes small-medium sized molecules
- Continuous hemofiltration
- Removes fluid by convection
- No dialysate, needs replacement fluid
- Removes large sized molecules
- Continuous hemodiafiltration
- Removes fluid by diffusion and convection
- Uses dialysate and replacement fluid
- Continuous hemodialysis
What should non-nephrologists understand about daily management of patients on CVVH?
- CICU clinicians should frequently communicate fluid balance and hemodialysis goals with nephrology and nurses
- The circuit has 2 pumps: 1 to pull fluid, another to push fluid back
- Monitor daily pressure trends as deviations may implicate issues with the access
- Look at I/Os on the circuit to determine fluid balance
- Ask RN if filter is clotting off because this can cause blood loss anemia due to the amount of blood lost when the circuit needs to be changed
- Electrolyte management:
- After 1-2 days of normalizing hyperkalemia, try to keep potassium steady using a 4 K bath
- CRRT can drop phosphorous precipitously, which may cause cardiac myocyte dysfunction; add Na-Phos if necessary.
- Very important: frequent line checks to identify infections. If the line is in for several days and begin considering a switch to a tunneled dialysis catheter, especially if longer-term RRT is expected.
How does the CICU team monitor for native renal recovery and initiate cardiovascular GDMT?
- The CICU team should assess daily trends in urine output. Patients may spontaneously make more urine especially as critical illness resolves. Consider trialing diuretics (FST) to assess recovery. Once hemodynamics improves, transition to iHD if there is still a persistent indication for RRT. Temporary dialysis lines are infection prone; consider exchanging for a tunneled iHD line if in place >1 week.
- Many GDMT medications, often crucial for CV optimization, are considered nephrotoxic and may increase serum potassium. Therefore, it is important to be thoughtful about timing of initiation.
- Consider initiating GDMT when the Cr is trending towards baseline. Cr is “cosmetic”, and the team should tolerate some Cr increases with life-saving GDMT. Please note that trends in potassium levels is more important than Cr with “nephrotoxic” CV meds.
- There may be a role for gastrointestinal potassium binders to facilitate GDMT optimization, but the clinical safety and efficacy remains unanswered (trials are underway).
- It is crucial for patients to get back on GDMT for improved long term cardiac outcomes.
References
- Gaudry S, Hajage D, Schortgen F, et al. Initiation strategies for renal-replacement therapy in the intensive care unit. New England Journal of Medicine. 2016;375(2):122-133.
- STARRT-AKI Investigators, Canadian Critical Care Trials Group, Australian and New Zealand Intensive Care Society Clinical Trials Group, et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383(3):240-251.
- Zarbock A, Kellum JA, Schmidt C, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the elain randomized clinical trial. JAMA. 2016;315(20):2190.
- Gaudry S, Hajage D, Martin-Lefevre L, et al. Comparison of two delayed strategies for renal replacement therapy initiation for severe acute kidney injury (AKIKI 2): a multicentre, open-label, randomised, controlled trial. The Lancet. 2021;397(10281):1293-1300.
- Chawla LS, Davison DL, Brasha-Mitchell E, et al. Development and standardization of a furosemide stress test to predict the severity of acute kidney injury. Crit Care. 2013;17(5):R207.
- Rabindranath K, Adams J, Macleod AM, Muirhead N. Intermittent versus continuous renal replacement therapy for acute renal failure in adults. Cochrane Database Syst Rev. 2007;(3):CD003773.





