Podcast: Embed
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | Pandora | iHeartRadio | Blubrry | TuneIn | Deezer | RSS
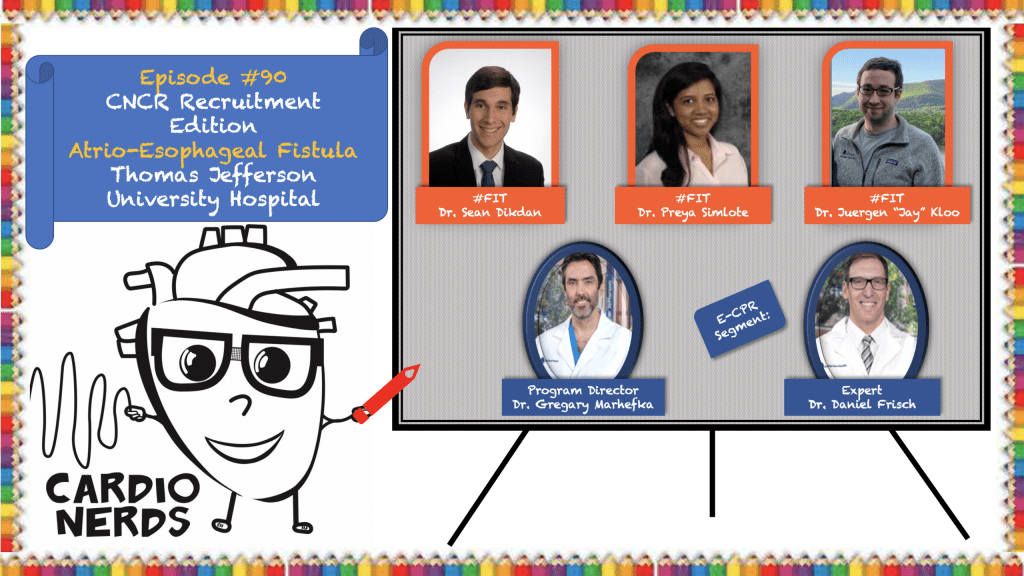
CardioNerds (Amit Goyal) joins Thomas Jefferson cardiology fellows (Jay Kloo, Preya Simlote and Sean Dikdan – host of the Med Lit Review podcast) for some amazing craft beer from Independence Beer Garden in Philadelphia! They discuss a fascinating case of atrioesophageal fistula (AEF) formation after pulmonary vein isolation (PVI). Dr. Daniel Frisch provides the E-CPR and program director Dr. Gregary Marhefka provides a message for applicants. Johns Hopkins internal medicine resident Colin Blumenthal with mentorship from University of Maryland cardiology fellow Karan Desai.
Jump to: Patient summary – Case media – Case teaching – References
The CardioNerds Cardiology Case Reports series shines light on the hidden curriculum of medical storytelling. We learn together while discussing fascinating cases in this fun, engaging, and educational format. Each episode ends with an “Expert CardioNerd Perspectives & Review” (E-CPR) for a nuanced teaching from a content expert. We truly believe that hearing about a patient is the singular theme that unifies everyone at every level, from the student to the professor emeritus.
We are teaming up with the ACC FIT Section to use the #CNCR episodes to showcase CV education across the country in the era of virtual recruitment. As part of the recruitment series, each episode features fellows from a given program discussing and teaching about an interesting case as well as sharing what makes their hearts flutter about their fellowship training. The case discussion is followed by both an E-CPR segment and a message from the program director.
CardioNerds Case Reports Page
CardioNerds Episode Page
CardioNerds Academy
Subscribe to our newsletter- The Heartbeat
Support our educational mission by becoming a Patron!
Cardiology Programs Twitter Group created by Dr. Nosheen Reza

Patient Summary
A man in his mid-60s with a history of paroxysmal Afib presented to the ED after one week of chest pain and altered mental status. His afib had been difficult to rate and rhythm control, and thus he had undergone catheter ablation with pulmonary vein isolation 3 weeks prior to presentation. In the ED he was found to be febrile and had a witnessed seizure. Blood cultures returned positive for Strep agalactiae and his CT head showed multiple areas of intravascular air. Join the Thomas Jefferson University Cardionerds as they take us through an expert discussion on the differential of post-catheter complications, the diagnosis of atrial-esophageal fistula and ultimately management of this potentially fatal complication!
Case Media
A. ECG: Normal sinus rhythm HR 105 bpm
B. CXR
C. CT head: Multiple tiny foci of air throughout bilateral cerebral hemispheres. Appearance is most suggestive of intravascular air, although it is unclear if it is venous, arterial or both.
D. MRI: 1. Restricted diffusion in bilateral cortical watershed zones, as well as in the posterior medial left cerebellar hemisphere, most consistent with recent infarctions.
E. CT Chest: A small focus of air tracking along the left mainstem bronchus anterior to the esophagus, may represent a small amount of pneumomediastinum versus air in an outpouching of the esophagus. No air tracking more cranially along the mediastinal soft tissues. No definite soft tissue defect in the esophagus.
F. Surgical repair of LA & Esophagus
Episode Teaching
The CardioNerds 5! – 5 major takeaways from the #CNCR case
- What is a pulmonary vein isolation? What are the most common complications? When is catheter ablation indicated?
- The majority of Afib triggers come from areas where the pulmonary veins attach to the left atrium. Approximately 15-20% of patients undergoing ablation will have non-pulmonary vein triggers. Guided by this anatomic and pathophysiologic underpinning, electrical isolation and ablation of these areas helps prevent propagation of the Afib impulses. The most effective method for pulmonary vein isolation (PVI) is ablation of the PV antrum, areas located near the PV ostia, using an oval mapping catheter to confirm ablation of electrical activity from the PV ostia.
- Vascular access complications (e.g. hematoma, pseudoaneurysm) are the most common complications following PVI and occur in approximately 1-4% (KD: I think complication rate is lower in studies I’ve reviewed) cases. Most other complications occur in less than 1% of cases and include cardiac tamponade/perforation, TIA/stroke, PV stenosis, pneumonia, phrenic nerve palsy, gastric motility disorders, atrial-esophageal fistula, and death.
- There is some growing evidence that catheter ablation may be superior to medical management alone in certain symptomatic populations (e.g., HFrEF). However, in the recent CABANA trial, catheter ablation did not significantly reduce death, disabling stroke, or serious bleeding compared to medical management in all comers with new-onset or untreated symptomatic Afib.
- The 2020 ESC guidelines on AFib give a Class I recommendation to Afib ablation for (1) symptom control in patients with paroxysmal or persistent AFib who have failed or are intolerant of at least one Class I or III antiarrhythmic drug (AAD); or (2) to reverse LV dysfunction in AFib patients when tachycardia-induced cardiomyopathy is highly probable regardless of their symptom status.
- What is an atrial esophageal fistula (AEF) and how does it form after a PVI?
- Esophageal perforation is a rare complication of PVI and occurs in 0.1-0.25% of procedures. If it goes undetected, an AEF can form, which is an abnormal connection between the esophagus and the left atrium. Overall it is the 2nd most common cause of death after PVI, with acute cardiac tamponade being the most common.
- In normal human anatomy, the esophagus runs just posterior to the LA, often coming within a few millimeters at its closest point. Regardless of modality (e.g. cryoablation, radiofrequency ablation), this close proximity can lead to damage of the esophagus via multiple mechanisms. First, all current ablation techniques use thermal injury, which can lead to direct mucosal damage the esophagus. Additionally, damage to the anterior esophageal plexus can impact gastric motility and emptying, which can increase reflux and lead to esophageal ulceration. Finally, thermal damage to the end arterioles can cause ischemic injury to the esophagus, which weakens the esophagus and predisposes it to ulcer and fistula formation.
- Though data is limited, ulceration of the esophagus appears to be the primary defect in AEF with the ulcer slowly propagating from the esophagus through the pericardium to the LA, forming a one way connection from the esophagus to the LA.
- What can be done to help avoid AEF formation during a PVI? What risk factors put patients at high risk for AEF formation?
- Esophageal temperature monitoring is frequently implemented to help reduce the risk of esophageal damage. In the 2017 HRS-led expert consensus statement on ablation of AFib, three-quarters of the writing group members terminate ablation if they observe a 1 C or 2 C rise in temperature from baseline, or a recorded temperature of 39C-40C in their practice. Temperatures above 41C increase the risk of AEF formation. Many providers also prescribe a PPI to reduce gastric acid secretion, a possible contributor to esophageal damage, but this data is not based clinical trial data.
- Multiple systems including esophageal cooling devices and methods to move the esophagus away from the LA are under development, but none have substantial clinical data to warrant widespread use.
- Risk factors for AEF formation include RF ablation (though can be seen with all ablation energy sources), higher esophageal temperature, and higher energy delivery (longer contact time, higher power, increased contact force, larger catheter tip, and higher irrigation flow).
- What are the most common signs and symptoms of an AEF and how is it diagnosed?
- Since AEFs start as an esophageal ulcer that progresses to a fistula, AEF formation typically takes 1-6 weeks (mean 20 days) from the time of ablation. Many of the common signs and symptoms are nonspecific and include fever, fatigue, AMS, chest pain, nausea, vomiting, dysphagia, hematemesis, melena, and dyspnea. Common complications include sepsis from bacteria (generally gram-positive organisms) entering the blood stream from the esophagus and stroke from air emboli.
- CT with oral and IV contrast or MRI imaging of the esophagus are the most useful diagnostic modalities. Occasionally this can show contrast extravasation from the LA to the esophagus, but more commonly it will show air from the esophagus into the pericardial space. Barium swallow can also be helpful as it has a very high specificity, but unfortunately a low sensitivity. Blood cultures and head CT are often obtained given the symptoms that patients present with and increase clinical suspicion if they demonstrate bacteremia or air emboli. Importantly, once AEF is suspected, EGD is contraindicated as insufflation of the esophagus can lead to a large air embolus and stroke.
- How are AEFs treated? What is the prognosis?
- Early diagnosis and treatment of AEFs is crucial as mortality is 100% without treatment. Esophageal ulceration or even pericardial esophageal fistulas have significantly better prognosis, highlighting the necessity for early identification. Esophageal stenting has not shown to be effective, and surgical repair with primary repair of the esophagus is the gold standard. Broad spectrum antibiotics should be utilized to treat or prevent the development of bacteremia and sepsis.
- Even with early identification and proper treatment, mortality is still very high with up to ~40% of patients dying after surgery.
References
- Arruda, M. S., Armaganijan, L., Biase, L. D., Rashidi, R., & Natale, A. (2009). Feasibility and Safety of Using an Esophageal Protective System to Eliminate Esophageal Thermal Injury: Implications on Atrial-Esophageal Fistula Following AF Ablation. Journal of Cardiovascular Electrophysiology, 20(11), 1272–1278. https://doi.org/10.1111/j.1540-8167.2009.01536.x
- Asad Zain Ul Abideen, Yousif Ali, Khan Muhammad Shahzeb, Al-Khatib Sana M., & Stavrakis Stavros. (2019). Catheter Ablation Versus Medical Therapy for Atrial Fibrillation. Circulation: Arrhythmia and Electrophysiology, 12(9), e007414. https://doi.org/10.1161/CIRCEP.119.007414
- Barbhaiya, C. R., Kumar, S., John, R. M., Tedrow, U. B., Koplan, B. A., Epstein, L. M., Stevenson, W. G., & Michaud, G. F. (2015). Global survey of esophageal and gastric injury in atrial fibrillation ablation: Incidence, time to presentation, and outcomes. Journal of the American College of Cardiology, 65(13), 1377–1378. https://doi.org/10.1016/j.jacc.2014.12.053
- Bunch, T. J., & Cutler, M. J. (2015). Is pulmonary vein isolation still the cornerstone in atrial fibrillation ablation? Journal of Thoracic Disease, 7(2), 132–141. https://doi.org/10.3978/j.issn.2072-1439.2014.12.46
- Calkins, H., Hindricks, G., Cappato, R., Kim, Y.-H., Saad, E. B., Aguinaga, L., Akar, J. G., Badhwar, V., Brugada, J., Camm, J., Chen, P.-S., Chen, S.-A., Chung, M. K., Nielsen, J. C., Curtis, A. B., Davies, D. W., Day, J. D., d’Avila, A., Groot, N. M. S. (Natasja) de, … Yamane, T. (2017). 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm, 14(10), e275–e444. https://doi.org/10.1016/j.hrthm.2017.05.012
- Chavez, P., Messerli, F. H., Dominguez, A. C., Aziz, E. F., Sichrovsky, T., Garcia, D., Barrett, C. D., & Danik, S. (2015). Atrioesophageal fistula following ablation procedures for atrial fibrillation: Systematic review of case reports. Open Heart, 2(1), e000257. https://doi.org/10.1136/openhrt-2015-000257
- Cummings Jennifer E., Schweikert Robert A., Saliba Walid I., Burkhardt J. David, Brachmann Johannes, Gunther Jens, Schibgilla Volker, Verma Atul, Dery MarkAlain, Drago John L., Kilicaslan Fethi, & Natale Andrea. (2005). Assessment of Temperature, Proximity, and Course of the Esophagus During Radiofrequency Ablation Within the Left Atrium. Circulation, 112(4), 459–464. https://doi.org/10.1161/CIRCULATIONAHA.104.509612
- Dagres, N., & Anastasiou-Nana, M. (2011). Prevention of atrial–esophageal fistula after catheter ablation of atrial fibrillation. Current Opinion in Cardiology, 26(1), 1–5. https://doi.org/10.1097/HCO.0b013e328341387d
- De Greef, Y., Ströker, E., Schwagten, B., Kupics, K., De Cocker, J., Chierchia, G.-B., de Asmundis, C., Stockman, D., & Buysschaert, I. (2018). Complications of pulmonary vein isolation in atrial fibrillation: Predictors and comparison between four different ablation techniques: Results from the MIddelheim PVI-registry. EP Europace, 20(8), 1279–1286. https://doi.org/10.1093/europace/eux233
- January Craig T., Wann L. Samuel, Calkins Hugh, Chen Lin Y., Cigarroa Joaquin E., Cleveland Joseph C., Ellinor Patrick T., Ezekowitz Michael D., Field Michael E., Furie Karen L., Heidenreich Paul A., Murray Katherine T., Shea Julie B., Tracy Cynthia M., & Yancy Clyde W. (2019). 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation, 140(2), e125–e151. https://doi.org/10.1161/CIR.0000000000000665
- Kapur Sunil, Barbhaiya Chirag, Deneke Thomas, & Michaud Gregory F. (2017). Esophageal Injury and Atrioesophageal Fistula Caused by Ablation for Atrial Fibrillation. Circulation, 136(13), 1247–1255. https://doi.org/10.1161/CIRCULATIONAHA.117.025827
- Mark, D. B., Anstrom, K. J., Sheng, S., Piccini, J. P., Baloch, K. N., Monahan, K. H., Daniels, M. R., Bahnson, T. D., Poole, J. E., Rosenberg, Y., Lee, K. L., Packer, D. L., & for the CABANA Investigators. (2019). Effect of Catheter Ablation vs Medical Therapy on Quality of Life Among Patients With Atrial Fibrillation: The CABANA Randomized Clinical Trial. JAMA, 321(13), 1275. https://doi.org/10.1001/jama.2019.0692
- Nair, G. M., Nery, P. B., Redpath, C. J., Lam, B.-K., & Birnie, D. H. (2014). Atrioesophageal Fistula in the Era of Atrial Fibrillation Ablation: A Review. Canadian Journal of Cardiology, 30(4), 388–395. https://doi.org/10.1016/j.cjca.2013.12.012
- Scanavacca, M. I., D’ávila, A., Parga, J., & Sosa, E. (2004). Left Atrial–Esophageal Fistula Following Radiofrequency Catheter Ablation of Atrial Fibrillation. Journal of Cardiovascular Electrophysiology, 15(8), 960–962. https://doi.org/10.1046/j.1540-8167.2004.04083.x
- Singh, S. M., d’Avila, A., Singh, S. K., Stelzer, P., Saad, E. B., Skanes, A., Aryana, A., Chinitz, J. S., Kulina, R., Miller, M. A., & Reddy, V. Y. (2013). Clinical outcomes after repair of left atrial esophageal fistulas occurring after atrial fibrillation ablation procedures. Heart Rhythm, 10(11), 1591–1597. https://doi.org/10.1016/j.hrthm.2013.08.012



















