Podcast: Embed
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | Pandora | iHeartRadio | Blubrry | TuneIn | Deezer | RSS
CardioNerd Amit Goyal, cardioobstetrics series co-chair Dr. Natalie Stokes, and episode lead Dr. Daniela Crousillat discuss normal cardiovascular physiology in pregnancy with Dr. Garima Sharma, Director of the Cardio-Obstetrics Program and the Ciccarone Center ‘s Associate Director of Preventive Cardiology Education in the Division of Cardiology. They discuss physiology from conception to post-partum, including the key hemodynamic, hormonal, and structural changes associated with normal pregnancy in the absence of pre-existing cardiovascular disease. Series introduction by Dr. Sharonne N. Hayes.
Claim free CME for enjoying this episode!
Abstract • Pearls • Quotables • Notes • References • Guest Profiles • Production Team
Episode Abstract
Join us for a thrilling ride with our expert as we dive into the normal cardiovascular physiology of women through pregnancy. We discuss physiology from conception to post-partum, including the key hemodynamic, hormonal, and structural changes associated with normal pregnancy in the absence of pre-existing cardiovascular disease. We discuss how these physiologic changes manifest the history, physical exam, and key diagnostic testing (ECG, laboratory markers, and echocardiogram). Armed with these basic principles, we join Dr. Garima Sharma on patient consults to learn about potential signs and symptoms of cardiovascular disease in pregnancy and appropriate ways to risk stratify women with pre-existing or acquired cardiovascular disease in pregnancy. Importantly, we delve deeper into the importance of the growing field of cardio-obstetrics in the context of rising maternal mortality and staggering racial disparities in the care and outcomes of women in pregnancy.
Pearls
- In normal pregnancy, plasma volume increases by up to 50% resulting in an adaptive decrease in systemic vascular resistance (SVR) by 25% and an increase in cardiac output (CO) by ~50% by the 2nd trimester.
- Brisk carotid upstrokes, an S3 gallop, soft systolic ejection murmurs, pedal edema, and a mildly elevated jugular venous pressure (JVP) can all be normal physiologic findings in pregnancy in the context of no other signs/symptoms to suggest heart failure.
- A normal NT-proBNP among pregnant patients with pre-existing cardiovascular disease has a high negative predictive value for predicting adverse maternal cardiac outcomes.
- Pregnancy risk predictor tools (mWHO, CARPREG II, ZAHARA) are a crucial component of pre-conception counseling to help predict which women with existing cardiovascular disease are at highest risk for adverse maternal outcomes.
- The U.S. ranks 1st in the world for maternal mortality among developed nations and cardiovascular disease is the leading cause of pregnancy-associated mortality in the U.S. Non-Hispanic Black are 3.5 times more likely to die from pregnancy as compared to White women.
Quotables
- “You don’t know where you are going until you know where you have been” – Dr. Garima Sharma on the importance of holding on to hope when encountering difficult situations in our training and career pathways.
- “Do not fear the pregnant patient! The pregnant patient is going through a normal physiologic process in her life, and the more we are familiar with it, the less we fear it” – Dr. Garima Sharma on taking care of pregnant patients.
- “If you are going to move the needle on maternal mortality and in making a long-term sustainable change in the lives of these women, you have to focus on prevention” – Dr. Garima Sharma on the importance of prevention in reducing maternal mortality.
- “Be empathetic. For most women, pregnancy is a normal state. These women need your help!” – Dr. Garima Sharma on the importance of taking care of women in pregnancy.
Show notes
- What are the normal hemodynamic changes that occur in pregnancy? Let’s talk physiology!
- Pregnancy, nature’s most grueling stress test, is a dynamic process associated with significant hemodynamic and physiological adaptations in the cardiovascular system which have evolved to support the needs of a developing fetus.
- Predictable and expected hemodynamic changes occur during pregnancy for all women. Healthy women can adapt without significant consequences, whereas in women with underlying cardiac conditions, these changes may unmask a previously unknown condition or exacerbate existing abnormal hemodynamics.
Adaptive Physiologic Changes of the Cardiovascular System (1)

- Plasma volume
- Increases by about 50-75% by the 2nd trimester of pregnancy to meet greater circulatory needs of placenta and maternal organs
- Erythropoietin causes an increase in red cell mass by 20-30% leading to relative dilution and “physiologic” anemia of pregnancy
- Systemic vascular resistance (SVR)
- To accommodate the increase in plasma volume, vasodilatation and vascular remodeling occur with a reduction in SVR
- SVR decreases starting early in the 1st trimester and falls by 25-30% in the 2nd trimester potentiated by progesterone and estrogen-induced vasodilatation
- Decreased SVR results in activation of the renal angiotensin-aldosterone system (RAAS) to maintain blood pressure and salt/water balance
- Cardiac output (CO)
- Increases by ~ 50% during pregnancy (up to 75% for a twin gestation!), starting at 5 weeks of gestation, and peaks at about 18-24 weeks in the 2nd trimester
- CO (stroke volume (SV) x heart rate (HR)) increases predominantly via an increase in SV, but also an increase in HR by about 10-15 bpm by the 3rd trimester due to activation of the sympathetic system
There are a multitude of other physiological changes that allow our cardiovascular systems to adapt to the normal hemodynamics of pregnancy.
- Respiratory: Increase in metabolic rate & O2 consumption, minute ventilation and tidal volume resulting in a mild compensatory respiratory alkalosis.
- Renal: Systemic vasodilation results in 50% increase in renal plasma flow and glomerular filtration rate (GFR), activation of RAAS to maintain fluid and electrolyte balance.
- Hematologic: “Physiologic” anemia of pregnancy due to increase in plasma volume > red blood cell mass, increased production of coagulation factors with promotion of a pro-thrombotic state.
- Endocrine: Increase in total cholesterol, triglycerides, LDL (by 50%) and decrease in HDL; mild insulin resistance.
Labor & Delivery and Post-Partum Period:
Labor:
- The maximum CO associated with pregnancy occurs during labor and immediately post-partum.
- Repeated Valsalva maneuvers with a doubling of CO (up to 10L!) in active labor
- Each uterine contraction displaces about 300-500 mL of blood back into the maternal systemic circulation
Post-partum:
- Immediate: Caval decompression from evacuation of gravid uterus leads to marked increase in venous return (“auto transfusion”) back into the maternal systemic circulation
- Two weeks post-partum: Maternal hemodynamics largely return to the pre-pregnancy state!
2. How are the normal physiological changes of pregnancy reflected in the physical exam and diagnostic cardiac testing? When should we worry?
- Physical Exam (2)
- Heart rate: Increases by 10-15 bpm by 3rd trimester, mild sinus tachycardia
- Blood pressure: Decrease of 10-15 mm Hg in both SBP and DBP, nadiring in 2nd trimester, improving to pre-pregnancy state in 3rd trimester
- Weight: 25-35 lbs considered normal total gestational weight gain in patients who are normal weight pre-partum
- Cardiac exam: Mildly elevated jugular venous pressure with more prominent x and y descents, brisk carotid upstrokes, soft, systolic ejection murmur (flow murmur), S3 gallop, mild pedal edema, varicose veins, mammary flow murmur
- ECG:
- Mild sinus tachycardia
- Infrequent premature atrial and ventricular atrial contractions
- Leftward axis deviation
- Q waves in inferior (II, III, aVF) and/or lateral (V4-V6) leads due to heart’s spatial shift left, anterior, and in the transverse plane to accommodate the gravid uterus
- Cardiac Biomarkers
- NT-proBNP
- Increase up to two-fold in pregnancy but should remain within normal range
- Important clinical utility in patients with pre-existing cardiac disease to serially assess changes throughout pregnancy
- BNP <100 pg/nL among women with cardiovascular disease has a 100% negative predictive value for identifying cardiac events during pregnancy (3)
- NT pro BNP <128 at 20 weeks has 97% NPV for maternal complications (4)
- NT-proBNP
- Echocardiography: (5)
- Increase in LV volumes (but remaining within normal limits) and 50% increase in LV and RV mass as response to increased blood volume and CO
- “Physiologic” left ventricular hypertrophy
- Left ventricular ejection fraction remains unchanged
- Mild increase in aortic root diameter
- Trivial MR, TR, and PR (not typically AR!)
- Trace, physiologic pericardial effusion (can be normal in up to 40%)
When should we worry?
- Diastolic murmurs
- Signs of congestive heart failure (crackles, elevated JVP/Kussmaul’s sign, marked lower extremity edema or weight gain)
- Loud P2 or RV heave which could signal elevated pulmonary pressures/pulmonary HTN
- Elevated NT-proBNP
- Large pericardial effusion or symptoms of pericarditis
3. What are the available pregnancy risk predictor scores for the risk stratification of women with pre-existing cardiovascular disease who are interested in achieving pregnancy?
Modified World Health Organization (mWHO) Classification (6)
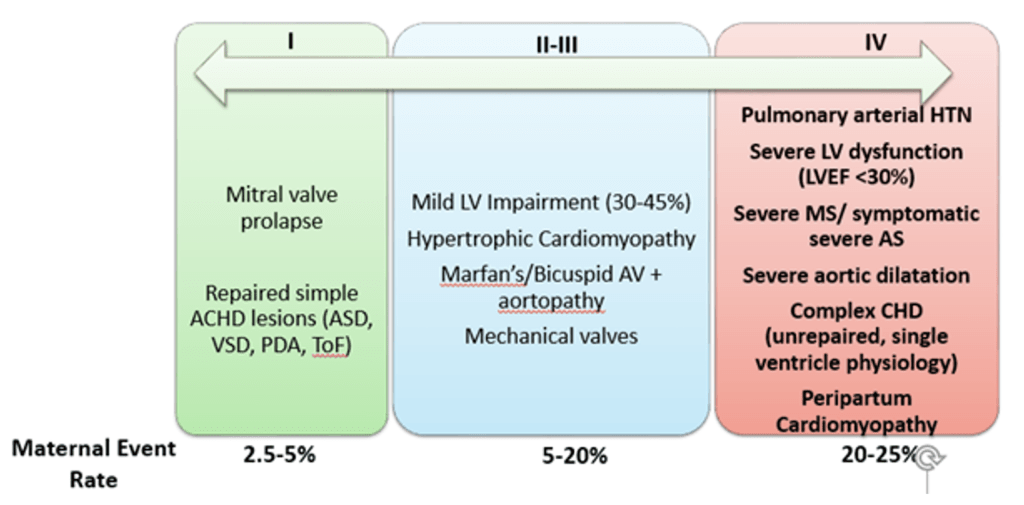
- Most commonly used risk prediction tool to estimate individual maternal cardiovascular risk in women with pre-existing CVD based on known cardiac pathology
- Classification ranges from simple lesions in Class I (mitral valve prolapse, repaired ASDs) to Class IV (pulmonary arterial hypertension, severe MS/AS, peripartum cardiomyopathy) in which pregnancy is typically advised against due to high (20-25%) maternal risk of adverse events
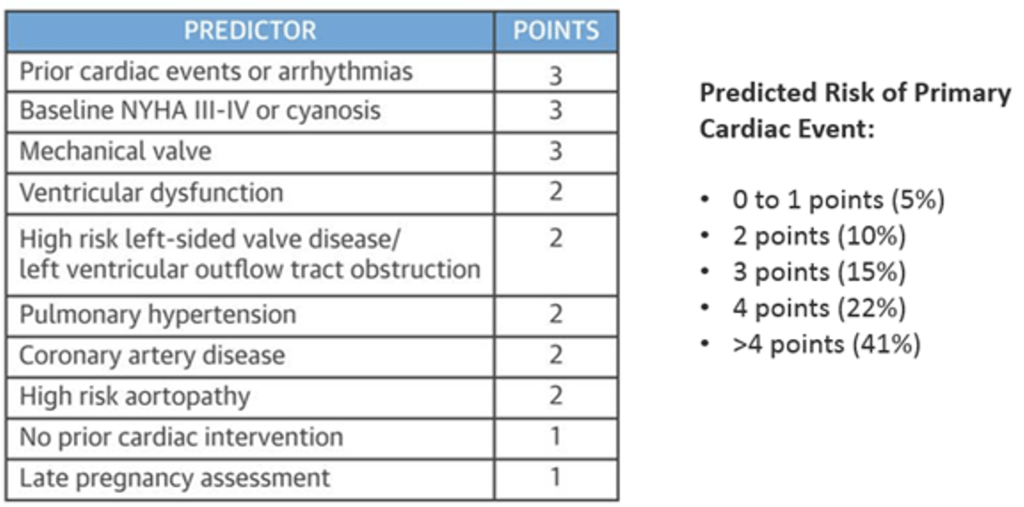
CARPREG (CArdiac Disease in PREGnancy Study) II Risk Score (7)
- Developed from the prospective Canadian Cardiac Disease in Pregnancy Study in women with pre-existing cardiac disease, the score includes 10 predictors of a cardiac event, including a prior history of cardiac events, baseline NYHA functional class, and late access to prenatal care to better determine overall risk (different than the mWHO classification which is based on just the cardiac lesion)
- Weight-based point system: 5% risk of complications in lowest risk group (0 to 1 points) versus >40% risk with > 4 points
ZAHARA Risk Score
- Weighted scoring system based on retrospective cohort of patients with pre-existing congenital heart disease only
- Least commonly used risk tool as based on limited patient population (ACHD)
4. What are the most common cardiac complications which can occur in women with pre-existing cardiovascular disease in pregnancy and when do they occur?
- Arrythmias: Atrial fibrillation is the most common arrythmia in women with underlying structural heart disease. PACs/PVCs can be common in normal pregnancy. If they occur, arrythmias are most common in the 2nd trimester.
- Heart failure: Worsening/decompensation of left ventricular function, particularly in women with personal or family history of cardiomyopathy and history of peripartum cardiomyopathy. The development of heart failure and pulmonary edema are most common in the 3rd trimester or immediately (<1 week) post-partum. (7)
- Don’t forget about other adverse pregnancy outcomes (APOs) which are associated with long term cardiovascular complications! (8)
- Maternal Complications: Hypertensive disorders of pregnancy (i.e. pre-eclampsia), gestational diabetes
- Obstetrical/Fetal Complications: Preterm birth, small for gestational age infant
- Review Ep #18 with Dr. Martha Gulati and Ep #41 with Dr. Leslie Cho for more!
5. What is the state of maternal mortality in the U.S. compared to the rest of the world, and what is this rise in maternal mortality attributed to?
- The United States ranks 1st among developed nations in maternal mortality (9)
- Cardiovascular disease is the leading cause of pregnancy-associated mortality in the United States and has gradually increased over time (7 to 17 deaths per 100,000 live births from 1989-2017)
- Maternal mortality is attributed to 1) rising maternal age, 2) comorbid pre-existing conditions (HTN, diabetes, obesity), and 3) the growing number of women with congenital heart disease achieving childbearing age
- Increase in obesity (41% of U.S. population) and chronic hypertension are two of the most important preventable risk factors!
- Pre-pregnancy HTN has doubled among women in past decade and disproportionately affects rural communities and racial groups (10)
- Over 700 women a year die of complications related to pregnancy each year in the United States, and it is thought that about two-thirds of those deaths are preventable.
- Non-Hispanic Blacks and American Indian/Alaskan Native women are 3-4x more likely to die from a pregnancy-related cause compared to White women (11).

References
- Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation 2014;130:1003-8.
- Mehta LS, Warnes CA, Bradley E et al. Cardiovascular Considerations in Caring for Pregnant Patients: A Scientific Statement From the American Heart Association. Circulation 2020;141:e884-e903.
- Tanous D, Siu SC, Mason J et al. B-type natriuretic peptide in pregnant women with heart disease. J Am Coll Cardiol 2010;56:1247-53.
- Kampman MA, Balci A, van Veldhuisen DJ et al. N-terminal pro-B-type natriuretic peptide predicts cardiovascular complications in pregnant women with congenital heart disease. Eur Heart J 2014;35:708-15.
- Liu S, Elkayam U, Naqvi TZ. Echocardiography in Pregnancy: Part 1. Current cardiology reports 2016;18:92.
- Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Kardiologia polska 2019;77:245-326.
- Silversides CK, Grewal J, Mason J et al. Pregnancy Outcomes in Women With Heart Disease: The CARPREG II Study. J Am Coll Cardiol 2018;71:2419-2430.
- Søndergaard MM, Hlatky MA, Stefanick ML et al. Association of Adverse Pregnancy Outcomes With Risk of Atherosclerotic Cardiovascular Disease in Postmenopausal Women. JAMA cardiology 2020;5:1390-8.
- Pregnancy Mortality Surveillance System. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillancesystem.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Freproductivehealth%2Fmaternalinfanthealth%2Fpmss.html. Accessed January 18th, 2021.
- Cameron NA, Molsberry R, Pierce JB et al. Pre-Pregnancy Hypertension Among Women in Rural and Urban Areas of the United States. J Am Coll Cardiol 2020;76:2611-2619.
- Petersen EE, Davis NL, Goodman D et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths – United States, 2007-2016. MMWR Morbidity and mortality weekly report 2019;68:762-765.
Guest Profiles

Dr. Garima Sharma is an Assistant Professor of Medicine in the Division of Cardiology and Department of Medicine at Johns Hopkins University. She serves as Director of the Cardio-Obstetrics Program and the Ciccarone Center ‘s Associate Director of Preventive Cardiology Education in the Division of Cardiology. Her clinical and research interests are in CVD in pregnancy specifically adverse pregnancy outcomes and CV risks, hypertensive disorders of pregnancy, and gender equity.

Dr. Daniella Crousillat is an advanced echocardiography fellow at Massachusetts General Hospital in Boston, MA. She is interested in sex differences in valvular heart disease and pregnancy-associated CVD with a special focus on health disparities and the care of vulnerable patient populations.










