CardioNerds Journal Club is a monthly forum for CardioNerds to discuss and breakdown recent publications on twitter and are produced with a corresponding infographic and detailed blog post. For more information, check out the CardioNerds Journal Club Page. This Journal Club focuses on the ADVOR Trial.

Table of contents for the ADVOR Trial summary:



September 29, 2022
Acetazolamide in Acute Decompensated Heart Failure with Volume Overload
Wilfried Mullens, M.D., Ph.D., Jeroen Dauw, M.D., Pieter Martens, M.D., Ph.D., Frederik H. Verbrugge, M.D., Ph.D., Petra Nijst, M.D., Ph.D., Evelyne Meekers, M.D., Katrien Tartaglia, M.Sc., Fabien Chenot, M.D., Samer Moubayed, M.D., Riet Dierckx, M.D., Ph.D., Philippe Blouard, M.D., Pierre Troisfontaines, M.D., et al., for the ADVOR Study Group

Relevant Literature – ADVOR Trial
- Loop diuretics are the mainstay of acute decongestive therapy in patients with heart failure and volume overload, recommended by current guidelines recommend for use in acute decompensated heart failure. Though chronic diuretic therapy is not associated with reduced mortality, timely administration of diuretic therapy in hospitalized patients and diuresis to euvolemia are associated with improved outcomes.
- Some have proposed sequential diuretic therapy as a more effective decongestive strategy, particularly in diuretic-resistant volume overload; however, insufficient data currently supports this practice.

Relevant Guidelines – ADVOR Trial
- 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure
- “Diuretic treatment should be started with an initial IV dose of furosemide, or equivalent dose of bumetanide or torsemide, corresponding to 1-2 times the daily oral dose taken by the patient before admission.” (Class I LOE C)
- “If the diuretic response remains inadequate… concomitant administration of other diuretics acting at different sites, namely thiazides or metolazone or acetazolamide, may be considered. However, this combination requires careful monitoring of serum electrolytes and renal function.”
Study Rationale – ADVOR Trial
- The carbonic anhydrase inhibitor acetazolamide reduces renal tubular sodium reabsorption and has been proposed to augment the diuretic effect of co-administered loop diuretics.
- Small, observational studies have shown improvement in sodium excretion among patients receiving both loop diuretics and carbonic anhydrase inhibitors.
Objective – ADVOR Trial
To evaluate whether the addition of acetazolamide to standardized intravenous loop diuretic therapy improves successful decongestion rates among patients with acute decompensated heart failure.

Trial – ADVOR Trial
- 27 trial sites in Belgium
- 1:1 parallel-group randomization
- Double-blind
- Placebo-controlled
Intervention
- Acetazolamide 500 mg IV bolus or matched placebo was administered once daily immediately after randomization and during the next two days or until complete decongestion.
- Complete decongestion was defined as the absence of clinical signs of fluid overload other than trace edema.
- All participants had home diuretics stopped at randomization and subsequently received an IV loop diuretic at double the maintenance dose administered once daily immediately after randomization and then as a split dose separated by ≥ 6 hours on each of the subsequent two days.
- Acetazolamide or placebo was administered concurrently with the first dose of loop diuretics each day.
- Loop diuretic dose was escalated per protocol if cumulative urine output over the 30-48 hours following the initial diuretic dose failed to exceed 3.5 liters and signs of fluid overload were still present.
- Other heart failure medications, including neurohormonal blockade, were left unadjusted during the treatment phase of the study.
Enrollment Criteria

Outcomes
- Primary Outcome
- Successful decongestion, defined by an absence of signs of volume overload (i.e., no more than trace edema, no residual pleural effusion, and no residual ascites).
- Secondary Outcomes
- Composite of death from any cause or rehospitalization for heart failure within 3 months.
- Combined renal safety endpoint of doubling of baseline creatinine, ≥ 50% reduction in eGFR, or the initiation of renal replacement therapy.
Statistical Analysis
- Outcomes stratified by LV EF ≤ or > 40% and trial center.
- Goal enrollment of 519 participants to reach 80% power in detecting a difference of 10% in the number of participants achieving successful decongestion.
- Intention-to-treat protocol.


Participant Characteristics:
- N = 519 (enrollment target met)
- Acetazolamide group: n = 259
- Placebo group: n = 260
- Average age: 78.2 ± 8.9
- Male: 62.6%
- Race: 99% white
- Average systolic BP: 127 ± 21 mm Hg
- Median (IQR) home maintenance dose (furosemide equivalent)
- Acetazolamide group: 80 (40-120) mg
- Placebo group: 60 (40-100) mg
- LV EF ≤40%: 43.2%
- Mean (IQR) eGFR: 39 (29-52)

Outcomes



Adverse Events
- Combined renal safety endpoint was met in 7 (2.7%) participants in the acetazolamide group compared to 2 (0.8%) in placebo group (P = 0.10)
- There were similar, low rates of hypokalemia and hypotension between groups
- Rates of adverse events related to placebo or acetazolamide during three months follow-ups were similar and low

Conclusions
- In this multicenter, randomized, placebo-controlled trial involving patients with acute decompensated heart failure and volume overload, the addition of acetazolamide to standardized intravenous loop-diuretic therapy was associated with a higher incidence of successful decongestion within three days after randomization and at discharge without increased risk of adverse events.
- Acetazolamide use was also associated with a decreased hospital stay.
Limitations & Considerations
- Although strong evidence shows incomplete decongestion at discharge is associated with worse outcomes, there was no significant difference in risk of death or rehospitalization between groups, even though the acetazolamide group had a higher rate of successful decongestion.
- Of note, the mortality rate in ADVOR was lower than that in DOSE and CARRESS-HF
- The trial results may not be generalizable to new diagnosis HF patients who are diuretic-naïve, given that diuretic-naïve patients were excluded from this trial.
- Important conclusions from subgroup analyses:
- Subgroup analysis suggests that acetazolamide is not superior among patients with a greater likelihood of diuretic resistance, including:
- Participants receiving > 60 mg of furosemide or equivalent as a home maintenance dose
- Participants who have ischemic cardiomyopathy, particularly with a reduced ejection fraction
- Participants who have eGFR ≥ 39 mL/min/1.73 m2
- The treatment effect for female participants was also non-significant in the subgroup analysis
- Subgroup analysis suggests that acetazolamide is not superior among patients with a greater likelihood of diuretic resistance, including:
- The trial was limited by suboptimal use of RAAS inhibitor (52.0%) and MRA (41.6%), as well as exclusion of patients using SGLT2i, given that these medications were not approved for HF when the trial was initiated.Participants were nearly exclusively white, with minimal racial and ethnic diversity, which may limit the generalizability of these findings. Future trials should seek greater diversity in enrollment.

- Mullens, Wilfried, et al. “Rationale and design of the ADVOR (Acetazolamide in Decompensated Heart Failure with Volume Overload) trial.” European journal of heart failure 20.11 (2018): 1591-1600.
- Felker, G. Michael, et al. “Diuretic strategies in patients with acute decompensated heart failure.” New England Journal of Medicine 364.9 (2011): 797-805.
- Bart, Bradley A., et al. “Ultrafiltration in decompensated heart failure with cardiorenal syndrome.” New England Journal of Medicine 367.24 (2012): 2296-2304.
- Matsue, Yuya, et al. “Time-to-furosemide treatment and mortality in patients hospitalized with acute heart failure.” Journal of the American College of Cardiology 69.25 (2017): 3042-3051.
- Verbrugge, Frederik H., et al. “Acetazolamide to increase natriuresis in congestive heart failure at high risk for diuretic resistance.” European journal of heart failure 21.11 (2019): 1415-1422.
- McDonagh, Theresa A., et al. “2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC.” European heart journal 42.36 (2021): 3599-3726.
- Mullens, Wilfried, et al. “Rationale and design of the ADVOR (Acetazolamide in Decompensated Heart Failure with Volume Overload) trial.” European journal of heart failure 20.11 (2018): 1591-1600.

The published archive features curated twitter highlights from the journal club event.

SUMMARY:
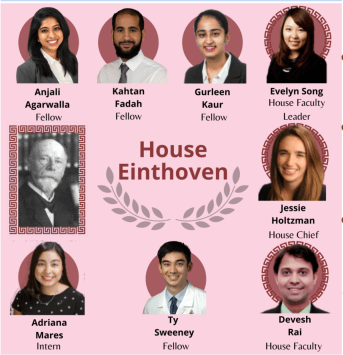
Dr. Ty Sweeney, Internal medicine resident, Johns Hopkins Bayview Medical Center
VISUAL ABSTRACT:
Dr. Gurleen Kaur, Internal medicine resident, Brigham Women’s Hospital
JOURNAL CLUB PROMO GRAPHIC:
Student doctor Adrianna Mares, medical student, The University of Texas at El Paso
Student doctor Chelsea Amo Tweneboah, medical student, St. George’s University,
TWEET PREPARATION:
Dr. Kahtan Fadah, Internal medicine resident, Texas Tech University
Dr. Anjali Agarwalla, Internal medicine resident, University of Pennsylvania
HOUSE JONES CHIEF FELLOW:
Dr. Jessie Holtzman, Chief resident, UCSF
HOUSE JONES FACULTY
Dr. Devesh Rai, @DeveshRaiMD, Cardiology fellow at Rochester General Hospital
DIRECTOR of JOURNAL CLUB:
Dr. Devesh Rai, @DeveshRaiMD, Cardiology fellow at Rochester General Hospital