CardioNerds Journal Club is a monthly forum for CardioNerds to discuss and breakdown recent publications on twitter and are produced with a corresponding infographic and detailed blog post. For more information, check out the CardioNerds Journal Club Page. This Journal Club focuses on the REVIVED-BCIS2 Trial.

Table of contents for the REVIVED-BCIS2 Trial summary:



August 27, 2022
Percutaneous Revascularization for Ischemic Left Ventricular Dysfunction
Divaka Perera, M.D., Tim Clayton, M.Sc., Peter D. O’Kane, M.D., John P. Greenwood, Ph.D., Roshan Weerackody, Ph.D., Matthew Ryan, Ph.D., Holly P. Morgan, M.B., B.Ch., Matthew Dodd, M.Sc., Richard Evans, B.A., Ruth Canter, M.Sc., Sophie Arnold, M.Sc., Lana J. Dixon, Ph.D., Richard J. Edwards, Ph.D., Kalpa De Silva, Ph.D., James C. Spratt, M.D., Dwayne Conway, M.D., James Cotton, M.D., Margaret McEntegart, Ph.D., Amedeo Chiribiri, Ph.D., Pedro Saramago, Ph.D., Anthony Gershlick, M.D., Ajay M. Shah, M.D., Andrew L. Clark, M.D., and Mark C. Petrie, M.D., for the REVIVED-BCIS2 Investigators

A presumed mechanism for the benefit of revascularization is the reversal of myocardial hibernation. Myocardial hibernation is an adaptive response that favors cardiomyocyte survival over contractile function.
Relevant Literature – REVIVED-BCIS2 Trial

Relevant Guidelines – REVIVED-BCIS2 Trial
2018 ESC/EACTS Guidelines on myocardial revascularization
- In patients with severe LV systolic dysfunction and CAD suitable for intervention, myocardial revascularization is recommended (Class I, LOE B).
- CABG is recommended as the first revascularization strategy choice in patients with multivessel disease and acceptable surgical risk (Class I, LOE B).
- In patients with one- or two-vessel disease, PCI should be considered as an alternative to CABG when complete revascularization can be achieved (Class IIa, LOE C).
- In patients with three-vessel disease, PCI should be considered based on the evaluation by the Heart Team of the patient’s coronary anatomy, the expected completeness of revascularization, diabetes status, and comorbidities (Class IIa, LOE C).
2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization
- In patients with SIHD and multivessel CAD appropriate for CABG with severe left ventricular systolic dysfunction (LVEF ≤ 35%), CABG is recommended to improve survival (Class I, LOE B-R).
- No recommendations regarding PCI for revascularization in severe LV systolic dysfunction.
Study Rationale – REVIVED-BCIS2 Trial
- Most randomized trials of coronary revascularization in patients with chronic coronary syndromes do not include patients with severe left ventricular dysfunction.
- Prevalence of heart failure due to LV systolic dysfunction is increasing.
- It is unclear if revascularization with PCI offers any incremental benefit over contemporary HF medications and device therapy.
Objective – REVIVED-BCIS2 Trial
To evaluate whether revascularization with PCI in addition to optimal medical therapy can improve event-free survival and left ventricular function in patients with severe ischemic left ventricular systolic dysfunction, as compared with optimal medical therapy alone.

Trial – REVIVED-BCIS2 Trial
REVIVED was a prospective, multicenter, randomized, open label trial. Although the trial was open label, researchers in charge of adjudication and analyses were blinded. Randomization was stratified by center in a 1:1 fashion.
Intervention
PCI plus optimal medical therapy (OMT) vs OMT alone
- OMT refers to individually adjusted pharmacotherapy with or without device intervention (i.e. AICD).
- In the PCI group, revascularization had to be attempted on ALL diseased proximal coronaries supplying viable myocardium
Enrollment Criteria

Outcomes
Primary Outcome:
- Composite of death from any cause or heart failure hospitalization
Secondary Outcomes:
Major
- LVEF at 6 and 12 months as measured by echocardiography
- Kansas City Cardiomyopathy Questionnaire (KCCQ) score
- EuroQol Group 5-Dimensions 5-Level Questionnaire score
- NYHA functional class
Other
- All-cause mortality
- HF hospitalization
- Cardiovascular mortality
- Appropriate ICD therapy
- Acute MI
- Unplanned revascularization
- Serial NT-pro-BNP
- Canadian Cardiovascular Society angina class
Statistical Analysis
- Follow up period: Minimum of 24 months
- Unadjusted time-to-event analyses with an intention to treat protocol
- Cox proportional hazard models were used to calculate hazard ratios and 95% confidence intervals
- Kaplan-Meier curves for cumulative incidence plotting

Participant Characteristics:
- Total sample size = 700
- PCI group = 347
- OMT group = 353
- Randomization yielded well-balanced trial groups with no significant differences at baseline
- Disproportionate representation of white male participants (88-93% white, 87-88% male)
- Approximately 70% of participants were NYHA class I or II vs approximately 30% NYHA class III or IV
- Approximately 40% with diabetes at baseline
- Approximately 70% active tobacco use
- Approximately 50-56% with history of prior MI
- Average LVEF at randomization: 27%
- Approximately 40% with 3-vessel coronary disease; 14% with left main coronary artery disease
Outcomes
Primary Outcomes
- There was no significant difference in the primary outcome between PCI group and controls: 37.2% vs 38%: HR 0.99 (95% CI 0.78 – 1.27).
- No benefit with PCI for primary outcome in all prespecified subgroups.
Secondary Outcomes:
Major
- LVEF at 6 and 12 months: No significant difference
- Kansas City Cardiomyopathy Questionnaire score: Favored PCI group at 6 and 12 months. Difference not significant at 24 months
- EuroQol Group 5-Dimensions 5-Level Questionnaire score (indexed): Favored PCI group at 6 and 12 months. Difference not significant at 24 months
- NYHA functional class: No significant difference
Other
- All-cause mortality: No significant difference
- HF hospitalization: No significant difference
- Cardiovascular mortality: No significant difference
- Acute MI: No significant difference

Adverse Events
- Unplanned revascularization: 2.9% in PCI group vs 10.5% in OMT group: HR0.27 (95% CI 0.13 – 0.53)
- Major bleeding
- At 1 year: 3.1% in PCI group vs 0.6% in OMT group: RR 4.95 (95% CI 1.09 – 22.43)
- At 2 years: No significant difference (3.4% vs 2.4%)

Conclusions
- The addition of revascularization by PCI to optimal medical therapy in patients with severe LV dysfunction and coronary artery disease but with viable myocardium did not significantly improve overall mortality or rates of heart failure hospitalization.
- PCI with OMT was not superior to OMT alone in improving LV systolic function, NYHA functional class, or quality of life.
Limitations & Considerations
- Few patients with anginal symptoms (66% with no angina and 32% with CCS angina class I/II)
- The results of the ISCHEMIA trial suggest PCI is not superior to OMT for management of stable CAD either
- Concordance between coronary arteries revascularized by PCI and viable myocardial segments has not been determined yet.
- The extent of CAD, in terms of anatomical location, stenosis severity, degree of ischemia, and functional significance, in the trial is not known. Data on rates of IVUS & OCT-guided PCI and rates of FFR/iFR measurement is still pending.
- There were fewer than anticipated occurrences of the primary outcome, though the hazard ratio of nearly 1.0 and bounds of the 95% CI suggest the risk of type II error is low
- Longer-term follow-up data is needed
Other Notes
- It should be noted that, in comparison to STICH, REVIVED had a higher rate of MRA and ARNI use, as well as higher proportion of patients with cardiac devices. For this reason, comparison of the two studies should be done with caution. Also, both trials differed in regards to inclusion/exclusion criteria and had approximately 10-year difference in mean age of participants.
- Between STICH and REVIVED, the cardiovascular mortality rates in the intervention groups were roughly similar at ~28% but the OMT group mortality rate in REVIVED was better than that in STICH. Are the positive results in STICH more of a function of the inferior OMT? Would STICH be positive if repeated today?
- However, cardiovascular mortality rates in the OMT group of REVIVED were still high: 24.9%.
- 53% of patients in REVIVED had prior MI, while 77% in STICH had prior MI.
- The REVIVED trialists did not report time since diagnosis of reduced systolic dysfunction.
- Is it plausible to think that myocardium experiencing relatively shorter “hibernation” periods may be more amenable to “waking up”?
- What is the role of viability testing? In STICH, myocardial viability was associated with LV systolic dysfunction but not long-term survival.

- Perera D, Clayton T, O’Kane P, et al. Percutaneous Revascularization for Ischemic Left Ventricular Dysfunction. N Eng J Med. 2022 Aug 27.
- Kirtane A. REVIVE-ing a Weak Heart. N Eng J Med. 2022 Aug 7.
- Perra D, Clayton T, Petrie M, et al. Percutaneous Revascularization for Ischemic Ventricular Dysfunction: Rationale and Design of the REVIVED-BCIS2 Trial: Percutaneous Coronary Intervention for Ischemic Cardiomyopathy. JACC Heart Fail. 2018 Jun;6(6):517-526.
- Cleland J, Calvert M, Freemantle N, et al. The Heart Failure Revascularisation Trial (HEART). Eur J Heart Fail. 2011 Feb;13(2):227-33.
- Beanlands R, Nichol G, Huszti E, et al. F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR-2). J Am Coll Cardiol. 2007 Nov 13;50(20):2002-12.
- Velazquez E, Lee K, Deja M, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Eng J Med. 2011 April 28; 364(17):1607-16.
- Velazquez E, Lee K, Jones R, et al. Coronary-Artery Bypass Surgery in Patients with Ischemic Cardiomyopathy. N Eng J Med. 2016 April 21;374(16):1511-20.
- Petrie M, Jhund P, She L, et al. Ten-Year Outcomes After Coronary Artery Bypass Grafting According to Age in Patients With Heart Failure and Left Ventricular Systolic Dysfunction. Circulation. 2016 Nov 1;134(18):1314-1324.
- Ryan M, Morgan H, Petrie M, et al. Coronary revascularisation patients with ischaemic cardiomyopathy. Heart. 2021 Apr;107(8):612-618.
- Neumann F, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EATS Guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165
- Lawton J, Tamis-Holland Jacqueline, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e4-e17.

The published archive features curated twitter highlights from the journal club event.

SUMMARY:
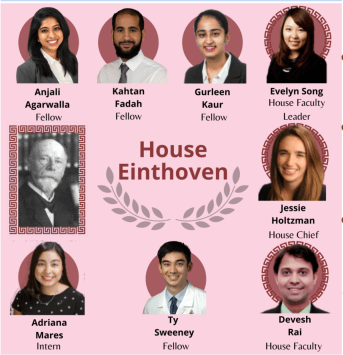
Dr. Gurleen Kaur, Internal Medicien Resident, Brigham Women’s Hospital
VISUAL ABSTRACT:
Dr. Anjali Agarwalla, Internal medicine resident, University of Pennsylvania
JOURNAL CLUB PROMO GRAPHIC:
Student doctor Adrianna Mares, medical student, The University of Texas at El Paso
Student doctor Chelsea Amo Tweneboah, medical student, St. George’s University,
TWEET PREPARATION:
Dr. Kahtan Fadah, Internal medicine resident, Texas Tech University
HOUSE JONES CHIEF FELLOW:
Dr. Jessie Holtzman, Chief resident, UCSF
HOUSE JONES FACULTY
Dr. Devesh Rai, @DeveshRaiMD, Cardiology fellow at Rochester General Hospital
DIRECTOR of JOURNAL CLUB:
Dr. Devesh Rai, @DeveshRaiMD, Cardiology fellow at Rochester General Hospital